Improving Patient Care Through Primary Care Provider Engagement
Written on
Chapter 1: The Importance of Primary Care
In the context of the American healthcare system, many individuals, possibly including yourself, may find that your primary care provider (PCP) oversees a patient panel of around 2,500 to 3,000 individuals, often conducting visits with 24 or more patients each day. This results in appointment times of about 20 minutes, with actual interaction often limited to just 10 to 12 minutes. Such brief consultations are typically insufficient, especially for patients managing multiple chronic conditions and a myriad of related challenges. To illustrate this, let’s examine a real-life case.
I previously introduced Henry; now, let's explore his situation in greater depth. Henry, a 69-year-old widower, resides alone in a rural area approximately 60 miles from a major city. He relies on a modest pension alongside Medicare, a Medigap policy, and a Medicare Part D drug plan. Recently, he faced a critical health crisis, being admitted to the ICU due to a severe urinary tract infection that escalated to his kidneys [pyelonephritis] and bloodstream [septicemia], culminating in acute respiratory distress syndrome. Thankfully, the intensive care he received was effective, and he survived.
A week after his discharge, Henry sought my advice regarding his medication regimen. He had been sent home with a new list of 23 different prescriptions, some taken multiple times daily, alongside a monthly injection. Unsure of the necessity of these medications, he reached out for clarity. While I couldn't act as his physician from 400 miles away, I offered to organize his medication list into categories and suggest pertinent questions for his doctor.
Henry later informed me that he had no dedicated primary care physician; instead, he consulted four different specialists for various health issues, with no communication between them. This lack of coordination often led to unnecessary prescriptions for blood pressure medications, contributing to his impotence and overall health complications.
This case exemplifies significant flaws in the current healthcare delivery system. Henry's four chronic conditions—heart failure, diabetes, hypertension, and depression—required cohesive management, ideally through a single PCP who understands his medical and personal circumstances.
The problems became evident when Henry was prescribed excessive medications without proper oversight, leading to adverse effects rather than effective treatment. The disjointed care he received is indicative of broader issues within the system, where uncoordinated care results in inflated costs and diminished quality.
Medicare readily funds extensive hospital care, like Henry's, which can amount to tens of thousands of dollars. In contrast, primary care physicians receive minimal compensation despite their crucial role in preventing such costly hospitalizations through proactive management.
I recommended that Henry find a dedicated primary care physician. He discovered a newly practicing doctor nearby and became one of the first patients. This PCP was able to devote the necessary time to Henry’s care, resulting in a significant reduction in his medications—from 23 to just seven—along with an improvement in his overall well-being and financial situation.
During our discussions, I learned that Henry weighed 285 pounds, having adopted a sedentary lifestyle after losing his wife. With little social interaction and a reliance on prepared foods, his diet was contributing to his health issues. We explored his meal choices, revealing concerning sodium levels in his canned soup, among other dietary missteps. Together, we devised a plan for healthier eating and regular physical activity.
After a few months, Henry reported a positive transformation. He began socializing at a local senior center, found new friendships, and even attended dances, which lifted his spirits. Although he still manages chronic illnesses, the comprehensive care from his PCP has led to improved health outcomes and a better quality of life.
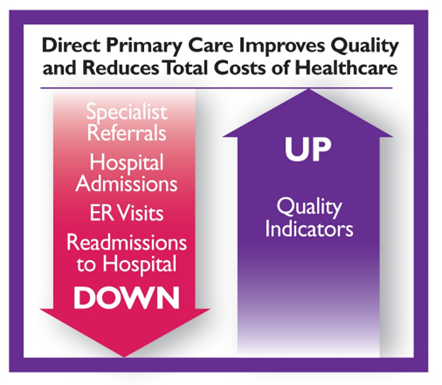
Henry’s experience underscores the necessity of having a committed primary care physician who can provide holistic care. Unfortunately, many PCPs face high overheads and low reimbursements, often leading to rushed visits. However, those who can invest time in patient care yield better health results. This brings us to the concept of Direct Primary Care (DPC), a model where patients pay their PCP directly, potentially lowering overall healthcare costs while enhancing care quality.
Here, we explore why having a Primary Care Provider is vital for patient health.
Chapter 2: Direct Primary Care as a Solution
In this chapter, we discuss the Direct Primary Care model and its benefits for patients.