Revolutionary Genetic Insights Could Transform Psychiatric Diagnosis
Written on
Chapter 1: Unraveling Psychiatric Disorders Through Genetics
Recently, I delved into a fascinating paper published in Cell, which details an extensive investigation into the genetic foundations of psychiatric disorders. The scale of this research is truly monumental, involving an analysis of genetic data from 750,000 individuals.
The research began as a comprehensive genome-wide association study, but its depth is astonishing. Researchers collected genomic information from 232,964 individuals diagnosed with psychiatric conditions. To put this into perspective, this equates to approximately two cities the size of New Haven. While major depression was the most prevalent diagnosis, a variety of other psychiatric conditions were also represented.
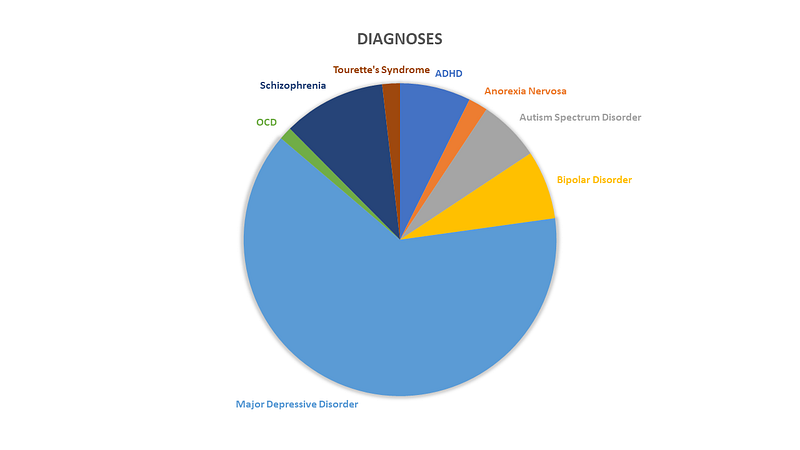
Additionally, the study included a control group of nearly 500,000 individuals, creating a substantial dataset. However, it's worth noting that this population was not as diverse as the actual New Haven, as all participants self-identified as being of European descent. This extensive sample enabled researchers to identify minor genetic variations more frequently found in those with psychiatric disorders.
In total, they discovered 136 genomic hotspots — represented as dots above the red dashed line in the accompanying Manhattan plot.
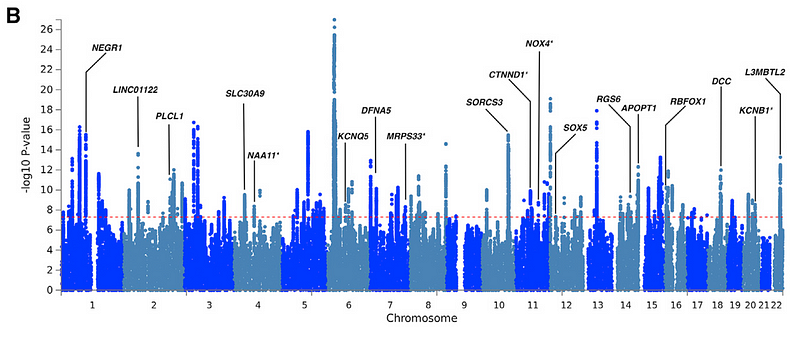
Among these, 35 hotspots had never been reported before, which is quite remarkable. However, the study's depth extends beyond just these findings. The researchers aimed to identify "pleiotropic loci" — genetic hotspots linked to multiple psychiatric disorders. This understanding may illuminate shared processes underlying various psychiatric illnesses and pave the way for more universal treatments.
Out of the 136 hotspots, 109 were identified as pleiotropic, showing associations with multiple disorders. This genetic interconnection allowed the researchers to create a network map illustrating how these diagnoses are genetically related.
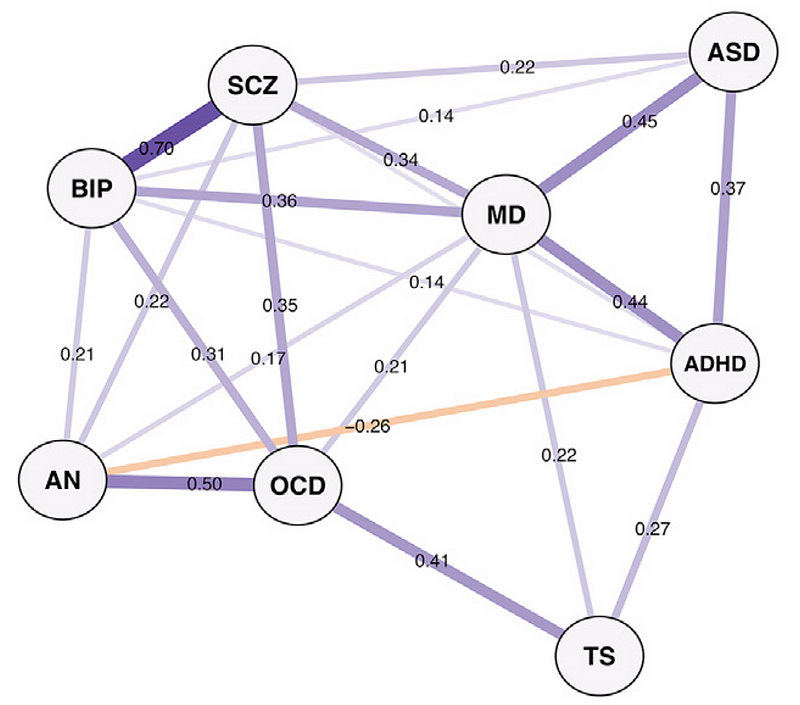
The map aligns closely with clinical observations: bipolar disorder and schizophrenia exhibit strong genetic ties, as do anorexia nervosa and obsessive-compulsive disorder. The established relationship between autism spectrum disorder and ADHD is expected, yet some emerging connections, like that between autism and major depression, warrant further investigation.
Interestingly, multiple bioinformatic methods highlighted three broad categories of disorders, potentially indicating underlying genetic processes. In the future, this research could reshape how we classify psychiatric conditions.
One hotspot, in particular, drew attention — a minor mutation in the DCC gene (known for its association with colon cancer) was found to be linked to all eight psychiatric diagnoses within the dataset.
While initially recognized for its connection to colon cancer, the DCC gene plays a crucial role in neurodevelopment by guiding axonal growth. Mutations that lead to loss of function in DCC can result in severe neurodevelopmental syndromes, often fatal during embryonic stages. The gene's altered function could contribute to a brain's susceptibility to environmental factors triggering psychiatric disorders.
Although targeting DCC may not eliminate psychiatric illnesses entirely, the insights gained from genetic studies could fundamentally alter our understanding of these conditions. This shift might alarm those preparing the next edition of the DSM, but ultimately, it could lead to better outcomes for patients.
The first video discusses the implications of the genetic study and its potential to reshape psychiatric understanding.
The second video explores how chronic diseases are influenced by gene expression, providing further context to the findings of the study.